HER2+ Breast Cancer Model Showdown: BT-474 vs. SK-BR-3, How to Choose?
Introduction
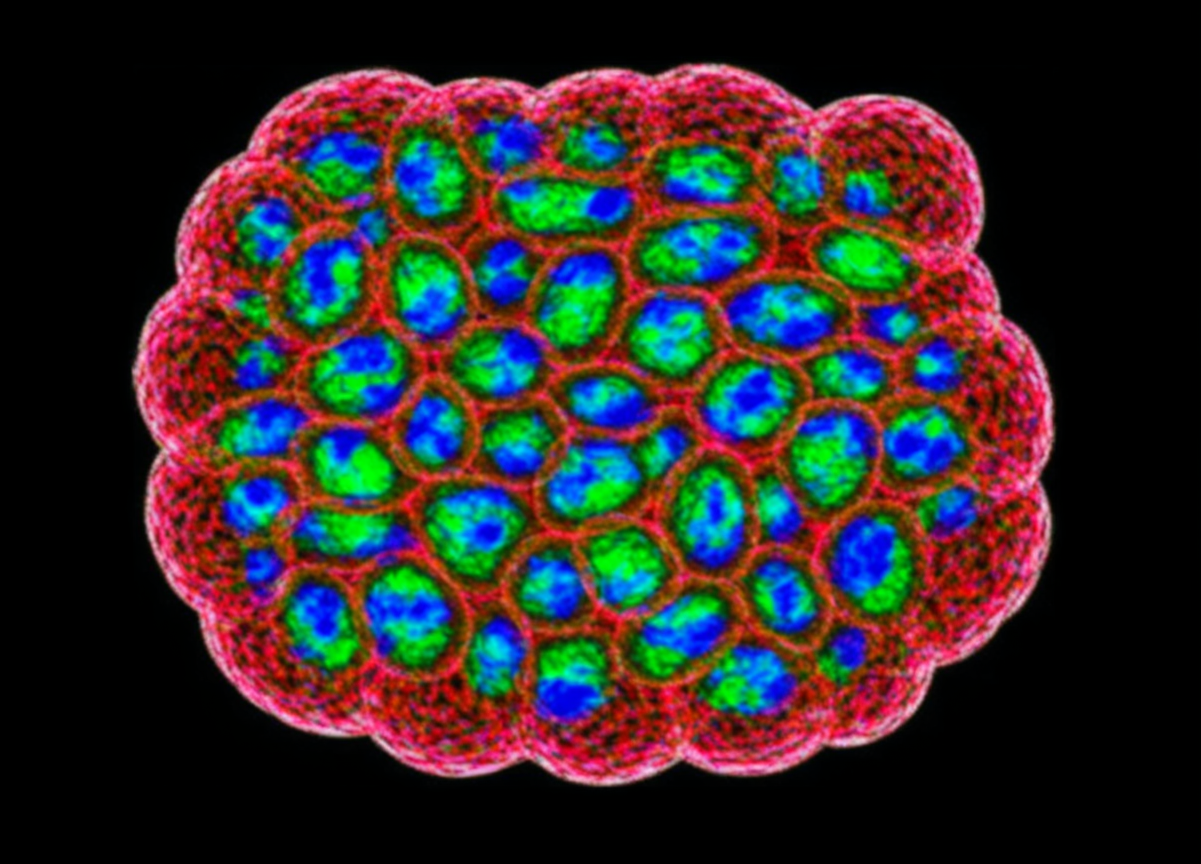
In the preclinical research of HER2-positive breast cancer, BT-474 and SK-BR-3 are two widely used, classic cell lines. Both are renowned for the amplification of the HER2 (also known as ERBB2) gene in their genome and the corresponding high expression of its protein, making them standard tools for testing various anti-HER2 therapies. However, despite sharing this critical feature, these two cell lines differ fundamentally in other important biological characteristics. The most central distinction is the status of the estrogen receptor (ER). This difference directly dictates the clinical subtypes they model and their most appropriate research applications. Therefore, understanding their similarities and differences is a prerequisite for designing rational experiments and correctly interpreting data.
Does your research involve HER2/ER pathway crosstalk? Choose our double-positive BT-474 cells, the ideal tool for studying combination therapies and endocrine resistance. Explore more>>
Hormone Receptor Status Dictates the Clinical Subtype Modeled
Breast cancer is a heterogeneous disease, classified into different subtypes based on the status of hormone receptors (HR, including ER and PR) and HER2. BT-474 and SK-BR-3 represent two distinct clinical branches within HER2-positive breast cancer.
BT-474: ER-Positive (ER+)
The BT-474 cell line co-expresses functional estrogen receptor (ER) and progesterone receptor (PR). This makes it a representative model for HER2+/HR+ double-positive breast cancer. Clinically, this is the most common subtype of HER2-positive breast cancer, accounting for about half of the cases. In such tumors, cell growth is driven not only by the HER2 signaling pathway but is also dependent on estrogen signaling. Complex signal crosstalk exists between these two pathways, which is a significant reason for treatment resistance, especially to endocrine therapy. Therefore, when the research question involves the following aspects, BT-474 is the mandatory choice:
1. Investigating the interaction between the HER2 and ER signaling pathways.
2. Evaluating the synergistic effects of combining endocrine therapy (e.g., tamoxifen) with anti-HER2 therapy (e.g., trastuzumab).
3. Exploring the molecular mechanisms of endocrine resistance in HER2+/ER+ tumors.
SK-BR-3: ER-Negative (ER-)
Unlike BT-474, SK-BR-3 cells do not express ER or PR. This establishes them as a representative model for HER2+/HR- breast cancer. In this type of tumor, cell growth and proliferation are driven almost exclusively by the overactive HER2 signaling pathway, without influence from estrogen signals. This provides a relatively "pure" research context. When the research goal is to focus on the HER2 signaling pathway itself, without interference from the ER pathway, SK-BR-3 is the superior choice. Applicable scenarios include:
1. Dissecting the downstream molecular events of the HER2 signaling pathway.
2. Screening and evaluating new drugs that only target HER2 (e.g., novel TKIs or ADCs) to assess their direct effects.
3. Serving as a clear positive control for comparing the potency of different anti-HER2 drugs.
Growth Characteristics and HER2 Expression Level
Beyond the decisive difference in ER status, these two cell lines also differ in their routine culture and certain molecular features, which can affect experimental handling and the interpretation of results.
Growth Characteristics:
BT-474 grows relatively slowly, with a doubling time of approximately 60-90 hours. In culture dishes, it tends to form tight, grape-like clusters (clumps), which makes cell digestion and the preparation of a single-cell suspension require more patience and skill.
SK-BR-3 grows relatively quickly, with a doubling time typically between 30-40 hours. Its cells are more dispersed in morphology and do not form large, difficult-to-handle clumps, making routine passaging, counting, and experimental setup more convenient.
HER2 Expression Level:
Both are HER2-high cell lines, which is the basis for their widespread use. However, quantitative analysis by Western Blot or flow cytometry has shown in most studies that the level of HER2 protein expression on the surface of SK-BR-3 cells is slightly higher than that of BT-474. This subtle difference may need to be considered in certain highly sensitive experiments. For instance, when developing an antibody-drug conjugate (ADC) that requires a certain HER2 density threshold for efficacy, a stronger response might be observed using SK-BR-3.
Recommended Application Scenarios| Scientific Goal | Primary Choice | Rationale |
|---|---|---|
| HER2/ER Pathway Crosstalk | BT-474 | ER-positive, models the double-positive subtype |
| Endocrine + Anti-HER2 Combo Therapy | BT-474 | Possesses both drug targets |
| "Pure" HER2 Signaling Pathway Study | SK-BR-3 | ER-negative, no interference from hormone signals |
| Experimental Convenience / Rapid Results | SK-BR-3 | Grows faster, more dispersed morphology |
| Assessing Dependence on Very High HER2 Expression | SK-BR-3 | HER2 expression level is typically highest |
Don't let cell culture be a barrier to your research. We provide low-passage, high-quality BT-474 cells with optimized handling tips to help you succeed. Buy now>>
Conclusion
In summary, choosing between BT-474 and SK-BR-3 is not a simple question of "which is better," but rather "which is more appropriate." The decision should always be centered around the specific scientific question. If your research aims to model the most common clinical subtype of HER2+/ER+ double-positive breast cancer and to explore complex signaling crosstalk and combination treatment strategies, then BT-474 is the only correct choice. Conversely, if your research requires a "pure" model with a clean background, rapid growth, and a focus on the HER2 signaling pathway itself, then SK-BR-3 will be the more efficient and suitable tool.
References
[1]Lasfargues, E. Y., et al. (1978). A new human breast carcinoma cell line (BT-474). In Vitro, 14(4), 353-353.
[2]Trempe, G., & Fogh, J. (1973). Variation in chromosome number of the SK-BR-3 human breast cancer cell line. Journal of the National Cancer Institute, 51(4), 1135-1143.
[3]Subik, K., et al. (2010). The integration of an estrogen receptor/c-myc signaling circuit provides a potential node for therapy in breast cancer. Cancer Research, 70(6), 2215-2225.
[4]Neve, R. M., et al. (2006). A collection of breast cancer cell lines for the study of functionally distinct cancer subtypes. Cancer Cell, 10(6), 515-527.