The GES-1 Cell Line: An In Vitro Model for Elucidating Helicobacter pylori Infection Mechanisms
Introduction
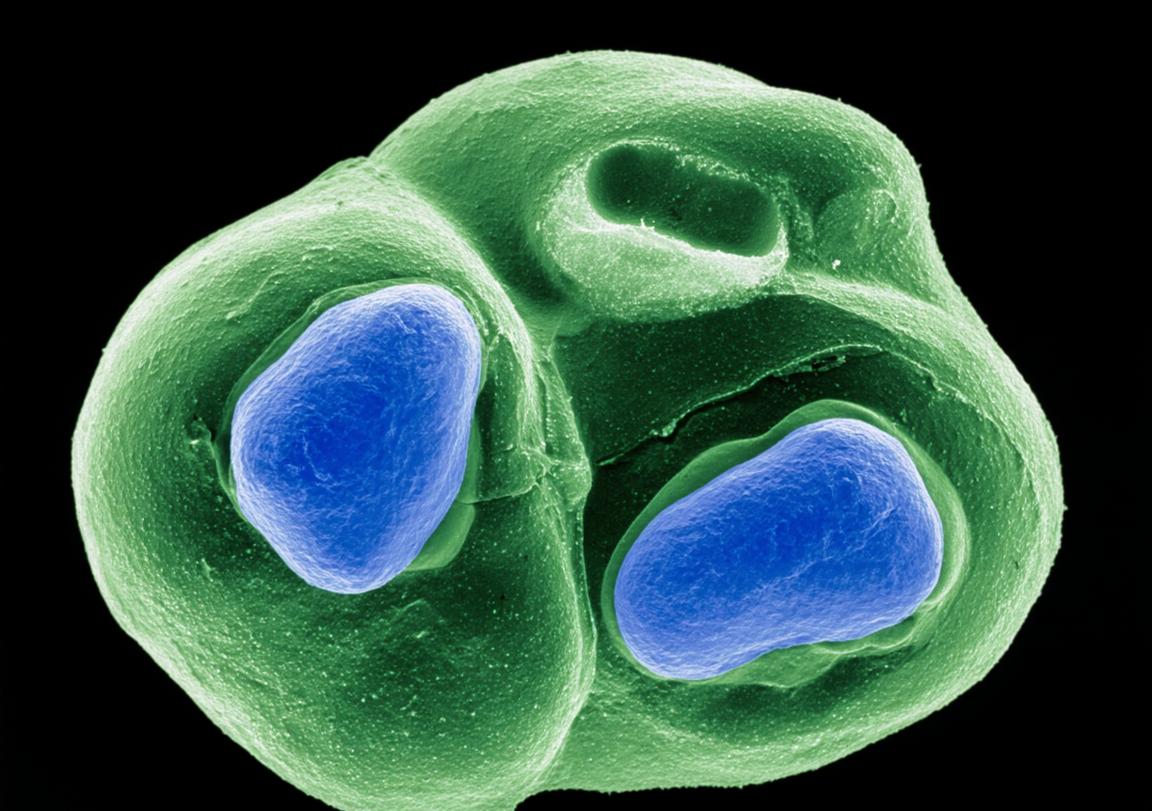
Helicobacter pylori is a Gram-negative bacterium capable of colonizing the human gastric mucosa and is a primary risk factor for chronic gastritis, peptic ulcers, and the development of gastric cancer. With approximately half of the global population infected, a deep understanding of its pathogenic mechanisms is crucial for developing effective prevention and treatment strategies. To investigate the complex interactions between the bacterium and its host cells in a controlled experimental setting, stable and reliable in vitro models are required. The human gastric epithelial GES-1 cell line, which is immortalized by SV40 T-antigen but is non-tumorigenic, closely mimics the biological characteristics of normal gastric epithelial cells. This makes it an ideal platform for simulating H. pylori infection and studying the host cellular response, leading to its widespread adoption by researchers globally. This article details four key applications of the GES-1 cell line in H. pylori infection research, demonstrating how it helps scientists unravel the pathogenic mysteries of this significant pathogen.
Build a stable and reproducible Helicobacter pylori infection model with ease. Choose GES-1 to accurately recapitulate the key interactions between the bacterium and host cells. Learn more>>
Simulating the Infection Process
The first step in studying H. pylori pathogenesis is to reconstruct the infection scenario in vitro. The GES-1 cell line provides an ideal host model for this purpose. In a typical experiment, GES-1 cells in their logarithmic growth phase are cultured in plates to form a monolayer, which is then co-cultured with a suspension of live H. pylori at a specific concentration. By setting different co-incubation times (usually from a few hours to 24 hours) and multiplicities of infection (MOI, the ratio of bacteria to cells), the dynamic process of infection can be precisely simulated. This co-culture system effectively recapitulates the critical step of H. pylori adhesion to the gastric epithelial cell surface and serves as the foundation for all subsequent mechanistic studies. Researchers can observe morphological changes in GES-1 cells following bacterial adhesion, such as the "hummingbird phenotype," which is a classic hallmark of the injection of the H. pylori virulence factor CagA into the host cell.
Analyzing Cellular Inflammatory Responses
Chronic inflammation is a central process through which H. pylori infection leads to mucosal damage and carcinogenesis. Upon infection with H. pylori, GES-1 cells initiate an innate immune response and secrete various inflammatory mediators, faithfully mimicking the in vivo inflammatory cascade. Among these, Interleukin-8 (IL-8) is the most extensively studied marker. IL-8 is a potent neutrophil chemoattractant, and its sustained high expression recruits a large number of immune cells to the site of infection, exacerbating inflammation. After infecting GES-1 cells with H. pylori, researchers can quantify the concentration of IL-8 protein in the culture supernatant using an Enzyme-Linked Immunosorbent Assay (ELISA) or measure the transcriptional level of IL-8 mRNA within the cells using Real-Time Quantitative PCR (RT-qPCR). Data consistently show that H. pylori infection significantly induces IL-8 production in GES-1 cells, and its expression level correlates positively with bacterial virulence and infection duration. This model has therefore become a standardized tool for assessing the inflammatory potential of different H. pylori strains and for screening anti-inflammatory drugs.
Studying the Effects of Bacterial Virulence Factors
The pathogenicity of H. pylori is largely determined by its virulence factors, with cytotoxin-associated gene A (CagA) and vacuolating cytotoxin A (VacA) being the two most important proteins. The GES-1 cell line offers an excellent platform to precisely dissect the function of these factors.
CagA is injected directly into the host cell cytoplasm via a specialized apparatus called the type IV secretion system (T4SS). Once inside GES-1 cells, CagA is phosphorylated by host kinases, subsequently interfering with cellular signaling, disrupting the cytoskeleton, and compromising cell-cell junctions. Using Western Blot analysis with specific antibodies, researchers can detect phosphorylated CagA in GES-1 cell lysates, directly confirming its successful translocation and activation.
VacA induces the formation of large acidic vacuoles within the host cell, leading to cellular dysfunction. By co-culturing GES-1 cells with purified VacA toxin or with VacA-secreting H. pylori, this characteristic vacuolation can be clearly observed under a light microscope. By creating H. pylori mutant strains with deletions in the cagA or vacA genes and comparing their effects to wild-type strains in the GES-1 model, scientists can definitively attribute specific cellular phenotypes to individual virulence factors, thereby uncovering their detailed mechanisms of action.
Screening for Anti-H. pylori Drugs or Natural Products
Building on the well-established infection models described above, the GES-1 cell line has become a vital platform for screening and evaluating potential therapeutic agents. Screening strategies typically focus on two outcomes: direct inhibition of the bacteria or protection of the host cells. In a drug screening experiment, candidate compounds (such as novel antibiotics, plant extracts, or probiotic metabolites) are added to the H. pylori-GES-1 co-culture system. The efficacy of the compound is then judged by assessing multiple endpoints. These can include measuring the viability of H. pylori to determine antibacterial activity, quantifying IL-8 secretion from GES-1 cells to assess anti-inflammatory effects, or evaluating cell viability (e.g., via an MTT assay) to measure the compound's protective effect against infection-induced damage. This comprehensive evaluation approach allows for the rapid and efficient screening of drug candidates with potential clinical value at the cellular level.
Need a reliable normal control for your gastric disease research? The GES-1 cell line provides a critical, non-tumorigenic baseline for your cancer and gastritis studies. Order now>>
Conclusion
In summary, the human gastric epithelial GES-1 cell line, as a stable, reliable, and near-physiological in vitro model, plays an indispensable role in H. pylori infection research. It is used not only to simulate the infection process and quantify inflammatory responses but also to precisely analyze the molecular functions of key virulence factors and to serve as an efficient platform for screening therapeutic candidates. Through the application of the GES-1 cell model, scientists have acquired a wealth of invaluable knowledge regarding H. pylori-host interactions. This knowledge will continue to provide a solid scientific foundation for developing new strategies to eradicate H. pylori infection and prevent gastric cancer.
References
[1]Li, N., et al. (2018). Helicobacter pylori CagA- and VacA-dependent pathways in the induction of the inflammatory response in human gastric epithelial cells. Frontiers in Cellular and Infection Microbiology, 8, 338.
[2]Wu, W., et al. (2020). Luteolin attenuates Helicobacter pylori-induced inflammation by inhibiting the Nrf2 and NF-κB signaling pathways. Helicobacter, 25(4), e12709.