The HEEC Cell Line: Building In Vitro Models for Endometriosis and Adenomyosis Research
Introduction
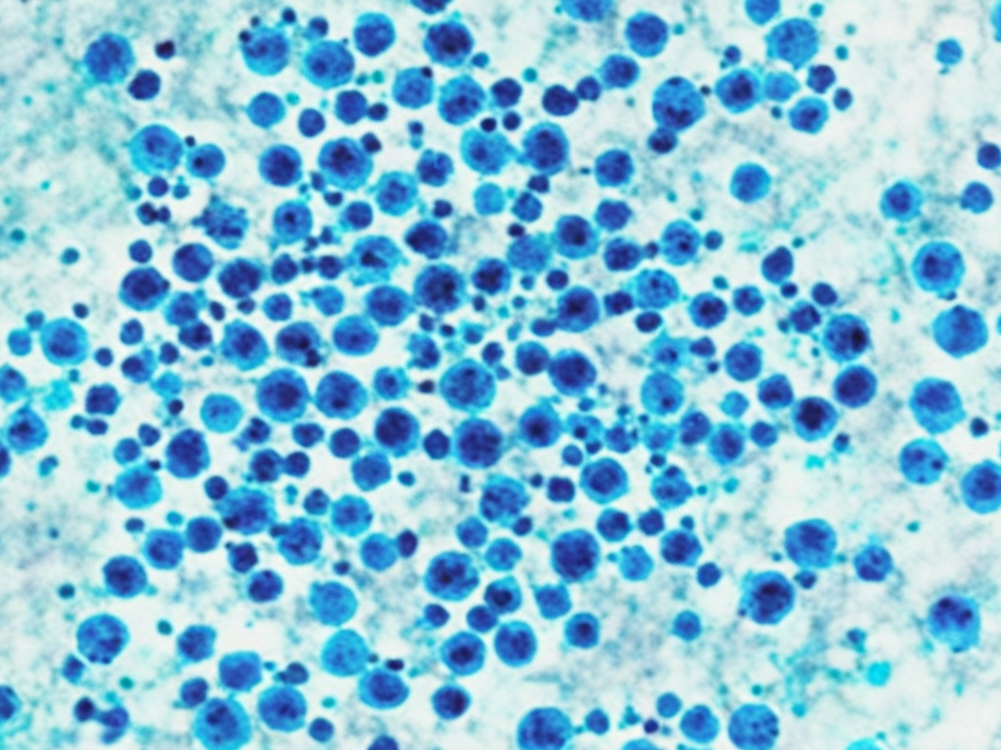
Endometriosis and adenomyosis are two common, estrogen-dependent gynecological diseases that severely impact the fertility and quality of life of millions of women worldwide. Their shared pathology involves the presence of endometrial-like tissue outside of the uterine cavity. Despite their high prevalence, the exact pathogenesis of these conditions remains incompletely understood, leading to limited treatment options that are often associated with side effects. To deeply explore the molecular mechanisms of these diseases and develop novel therapeutic strategies, researchers require a stable and reliable "normal" reference. The immortalized human endometrial epithelial cell line (HEEC) has become an indispensable research tool to meet this need.
Studying endometriosis? Our HEEC cells are your indispensable "normal" control to help you precisely identify disease-specific targets. Click to check>>
Comparative Studies of Abnormal Cell Adhesion and Invasion
The theory of retrograde menstruation is one of the most widely accepted hypotheses for the origin of endometriosis. It posits that menstrual blood containing viable endometrial fragments flows backward through the fallopian tubes into the pelvic cavity. For ectopic lesions to form, these fragments must successfully adhere to and invade the peritoneal lining. "Adhesion" and "invasion" are therefore critical initiating steps in this process.
The HEEC cell line plays a vital role as a "normal control" in such studies. It represents the behavior of normal, eutopic endometrial epithelial cells. Researchers can construct in vitro co-culture models, for instance, by seeding either HEEC cells or primary cells isolated from patients' endometriotic lesions onto a monolayer of peritoneal mesothelial cells (the cells lining the abdominal cavity). After a period of incubation, the number of adherent cells and their ability to invade the mesothelial layer can be quantitatively analyzed.
Numerous comparative studies have found that, compared to HEEC cells, endometrial cells from ectopic lesions exhibit significantly enhanced adhesive and invasive capabilities. This indicates that the ectopic cells have acquired an abnormal "aggressive" phenotype. Using HEEC as a baseline, scientists can further investigate which molecules (e.g., integrins, matrix metalloproteinases/MMPs) are aberrantly overexpressed in ectopic cells to mediate this hyper-adhesive and invasive behavior. This provides clear targets for the development of early intervention drugs aimed at blocking the "landing" of ectopic lesions.
Investigating Dysregulation of Inflammation and Hormone Response
Endometriosis is not just a disease of tissue misplacement but is also a chronic inflammatory condition. The ectopic lesions themselves produce and attract a large number of inflammatory cells and cytokines (such as TNF-α, IL-6, and IL-1β), creating a pro-inflammatory microenvironment that promotes lesion survival and growth.
The HEEC line provides a clear baseline for how normal endometrial epithelium responds to inflammatory stimuli. Researchers can treat HEEC cells with specific concentrations of inflammatory cytokines and analyze the resulting changes in gene expression profiles and protein secretion, thereby establishing a "normal response model." This model can then be compared to the response of cells derived from endometriotic lesions under the same stimuli. Studies have shown that the response of ectopic cells to inflammation is often exaggerated and dysregulated; they produce even more inflammatory mediators, creating a vicious cycle that perpetuates local inflammation.
Furthermore, progesterone resistance is another key pathological feature of endometriosis. Under normal conditions, progesterone inhibits the proliferation and promotes the differentiation of endometrial cells. However, ectopic lesions are insensitive to this suppressive effect. HEEC cells retain a normal response to progesterone. Therefore, by comparing the differences in proliferation, apoptosis, and the expression of related genes between HEEC and ectopic cells before and after progesterone treatment, the molecular mechanisms of progesterone resistance can be thoroughly investigated, providing a rationale for developing novel and more effective progestin-based therapies.
Screening for Specific, Targeted Therapeutic Drugs
Currently, the pharmacological treatment for endometriosis primarily relies on hormonal therapies that control the disease by suppressing ovulation or reducing estrogen levels. These treatments are often accompanied by side effects and have a high rate of recurrence upon discontinuation. Consequently, developing non-hormonal, more targeted drugs is a major focus of research in the field.
In this process, the HEEC cell line is an indispensable component for assessing drug safety and specificity. An ideal targeted drug should selectively inhibit the abnormal behaviors of ectopic lesion cells (e.g., excessive proliferation, invasion, inflammation) while having minimal impact on normal, eutopic endometrial cells. This selectivity is crucial to minimize interference with the normal menstrual cycle and fertility.
A typical drug screening workflow involves applying candidate compounds simultaneously to both ectopic endometrial cells and HEEC cells (as the normal control). Using high-throughput screening technologies, researchers can rapidly identify compounds that effectively inhibit the viability of ectopic cells at low concentrations but have little effect on the viability of HEEC cells. This differential effect, known as the "therapeutic window," is a key criterion for a candidate drug to advance to the next stage of preclinical research.
Need a stable, hormone-responsive model? Our HEEC cells retain a normal response to estrogen and progesterone, making them the ideal choice for your reproductive biology research. Order now>>
Conclusion
In summary, the HEEC cell line is more than just a simple cell culture; it is a fundamental reference standard in the field of endometriosis and adenomyosis research. By enabling systematic comparisons with cells derived from pathological lesions, HEEC allows researchers to precisely identify what is "abnormal" in the disease state, whether at the level of cell behavior, inflammatory response, or hormone signaling. More importantly, by acting as a "safety sentinel" in drug screening, it provides a solid scientific foundation for the development of more precise and safer therapies for the future.
References
[1]Kao, L. C., et al. (2003). Global gene profiling in human endometrium during the window of implantation. Endocrinology, 144(7), 2870-2881.
[2]Wotawa, C., et al. (2009). The role of the inflammatory mediators in endometriosis. Wiener Medizinische Wochenschrift, 159(21-22), 529-532.
[3]Burney, R. O., & Giudice, L. C. (2012). Pathogenesis and pathophysiology of endometriosis. Fertility and Sterility, 98(3), 511-519.
[4]Brosens, J. J., et al. (2009). Progesterone resistance in endometriosis: link to failure to undergo decidualization. Fertility and Sterility, 92(3), 859-864.