From In Vitro to In Vivo: Standardized Applications of the IOMM-Lee Cell Line in Developing Meningioma Xenograft Models
Introduction
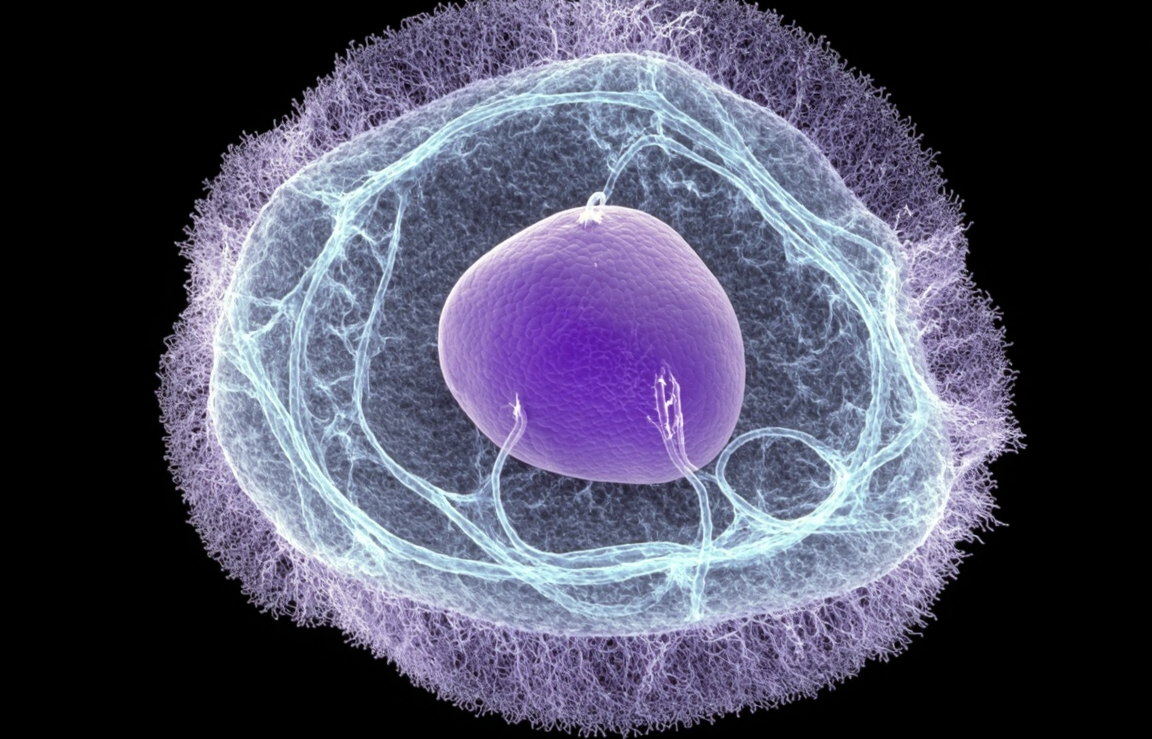
In the research and development of drugs for meningioma and the study of its pathological mechanisms, in vitro cell-based assays are fundamental. However, their results cannot fully predict outcomes within the complex environment of a living organism. To bridge the gap between laboratory research and clinical application, it is essential to establish animal models that can effectively mimic the tumor growth environment in humans. Xenograft models, which involve transplanting human tumor cells into immunocompromised animals, are a core technology for achieving this goal. The IOMM-Lee cell line, derived from a high-grade malignant meningioma, exhibits high proliferation and invasion capabilities, making it an ideal cell source for developing stable and reproducible meningioma xenograft models and a powerful tool for preclinical pharmacodynamic evaluation and pathological investigations.
Eliminate experimental variability from the start. We provide STR-authenticated, mycoplasma-free IOMM-Lee cells to give your research the most solid foundation. Order Now>>
The Subcutaneous Xenograft Model: A Convenient Tool for Primary Drug Screening
The subcutaneous xenograft model is one of the most fundamental and widely used approaches for developing meningioma animal models. Its procedure is relatively straightforward, it boasts a high rate of tumor formation, and the resulting tumors are easy to observe and measure. These features make it highly suitable for large-scale, preliminary drug screening and for studying tumor growth kinetics.
Model Establishment Protocol:
Cell Preparation: IOMM-Lee cells in their logarithmic growth phase are harvested and prepared into a single-cell suspension using trypsin. Cell viability is confirmed to be above 95% using a hemocytometer or automated cell counter. The cells are then resuspended in a serum-free medium or phosphate-buffered saline (PBS) to the desired concentration, typically 1×10⁶ to 5×10⁶ cells per mouse.
Animal Selection: 4-6 week-old immunocompromised mice, such as BALB/c nude or NOD/SCID mice, are commonly used to prevent immune rejection of the human tumor cells.
Injection Procedure: Under aseptic conditions, the cell suspension (usually 100-200 µL) is slowly injected subcutaneously into the flank of the mouse.
Tumor Monitoring: Tumor dimensions, including the length (L) and width (W), are measured 2-3 times per week using calipers. The tumor volume is then calculated using the formula V = 0.5 × L × W². The body weight and overall health of the mice are also monitored closely as indicators of systemic drug toxicity.
While this model is excellent for rapidly assessing the basic in vivo anti-tumor activity of drug candidates, its primary limitation is that the subcutaneous microenvironment differs significantly from the intracranial site of origin, failing to replicate key physiological structures like the blood-brain barrier.
The Orthotopic Intracranial Model: High Fidelity to Clinical Pathology
To more accurately simulate the growth environment and biological behavior of human malignant meningioma, researchers often establish orthotopic intracranial xenograft models. This model better recapitulates tumor-brain tissue interactions, local invasion, and penetration of the blood-brain barrier, giving it indispensable value in advanced preclinical studies.
Model Establishment Protocol:
Stereotactic Positioning: After being deeply anesthetized, the mouse is secured in a stereotactic frame. A small burr hole is drilled in the skull at predetermined coordinates.
Cell Injection: Using a microsyringe (e.g., a Hamilton syringe), a small volume of the IOMM-Lee cell suspension (typically 2-5 µL containing approximately 1×10⁵ cells) is injected very slowly into the subdural space or brain parenchyma. A slow injection rate is critical to prevent a sudden increase in intracranial pressure and reflux of the cell suspension.
Post-operative Care: After injection, the burr hole is sealed with bone wax, the scalp is sutured, and the mouse is kept warm and monitored until fully recovered from anesthesia.
Studies have demonstrated that tumors formed intracranially by IOMM-Lee cells exhibit histopathological features that closely resemble those of human high-grade meningiomas. These features include high cellularity, marked nuclear atypia, active mitosis, and invasive growth into adjacent brain tissue. This makes the orthotopic model an ideal platform for investigating mechanisms of tumor invasion and for evaluating the efficacy of drugs designed to cross the blood-brain barrier.
Non-invasive Monitoring of Tumor Growth
Traditionally, the assessment of intracranial tumor growth relied on observing the onset of neurological symptoms or on terminal histopathological examination, which precludes dynamic, continuous monitoring of tumor progression in the same animal. The advent of Bioluminescence Imaging (BLI) has revolutionized this process.
Application of the Technology:
Cell Line Engineering: First, IOMM-Lee cells are genetically engineered, typically using a lentiviral vector, to stably express a luciferase enzyme.
In Vivo Imaging: After the intracranial model is established, mice are periodically administered the luciferase substrate, D-luciferin, via intraperitoneal injection. The substrate is catalyzed by the enzyme in living tumor cells, producing light. This light signal is then captured by a highly sensitive in vivo imaging system (e.g., IVIS).
Data Analysis: The intensity of the light signal correlates directly with the number of viable tumor cells. By quantifying this photon flux, researchers can non-invasively, accurately, and longitudinally track tumor growth, stasis, or regression in response to therapy.
Empower your cutting-edge research. IOMM-Lee cells can be readily engineered for bioluminescence in vivo imaging. Click to check>>
BLI enables the longitudinal and quantitative monitoring of tumor burden, which not only significantly improves data accuracy and comparability but also aligns with the "3Rs" principles (Replacement, Reduction, Refinement) of animal welfare by reducing the total number of animals required for an experiment.
Conclusion
The IOMM-Lee cell line is a robust and reliable tool for establishing xenograft models of malignant meningioma. By utilizing a range of models—from the simple subcutaneous model suitable for high-throughput screening to the clinically relevant orthotopic intracranial model—and combining them with advanced non-invasive imaging technologies, researchers can create sophisticated, multi-layered preclinical research platforms. These models play a critical role in evaluating the efficacy of new drugs, investigating mechanisms of tumor invasion and metastasis, and optimizing therapeutic strategies, thereby significantly advancing the translation of basic meningioma research into clinical practice.
References
[1]Mandara, M. T., et al. (2010). IOMM-Lee: a new anaplastic meningioma cell line: histopathological and cytogenetic characterization. Journal of Neuro-Oncology, 96(3), 353–362.
[2]Stayman, J. W., et al. (2011). In vivo bioluminescence imaging of intracranial meningioma in a nude mouse model. Journal of Neuro-Oncology, 105(3), 501–508.