Accelerating Drug Discovery: How MHCC97-H-LUC Greenlights Anti-Hepatocellular Carcinoma Drug Screening
Introduction
The development of novel anti-cancer drugs is a race against time, yet traditional preclinical drug screening methods face significant bottlenecks. Conventional models that rely on endpoint analyses, such as tumor volume measurements or histopathology, are not only time-consuming and costly but also fail to capture the dynamic effects of a drug during treatment. This is particularly true when assessing the inhibition of tumor metastasis. Recently, molecular imaging techniques, led by Bioluminescence Imaging (BLI), have sparked a revolution. Among these, the MHCC97-H-LUC cell line stands out as a powerful tool, shining a "green light" on the screening and evaluation of anti-hepatocellular carcinoma (HCC) drugs and profoundly transforming the R&D paradigm.
Struggling with long drug evaluation cycles? Use MHCC97-H-LUC cells to accelerate your drug screening process by weeks. Order now>>
Establishing a Visual Pharmacodynamic Evaluation Model
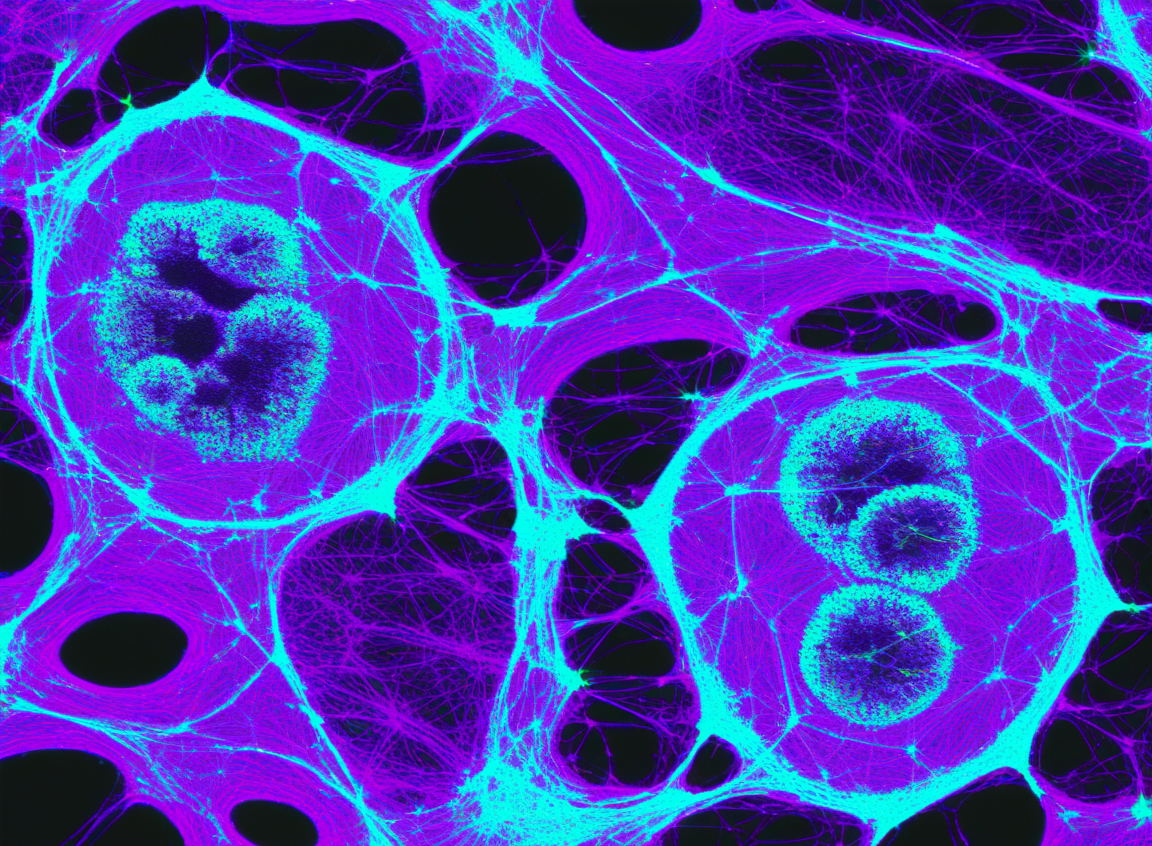
To accurately assess the anticancer potential of a candidate drug, a stable and reliable animal model that mimics in vivo tumor progression is essential. The advent of the MHCC97-H-LUC cell line makes the construction of this model both intuitive and efficient.
This cell line originates from the human HCC cell line MHCC97-H, which is known for its high metastatic potential. Scientists have stably integrated the luciferase (Luc) gene into its genome using techniques like lentiviral transduction. In a typical drug screening workflow, researchers inoculate a specific number of MHCC97-H-LUC cells into immunocompromised mice (e.g., subcutaneously or orthotopically in the liver). After several days or weeks, following an intraperitoneal injection of D-luciferin, the location and size of the tumors can be clearly visualized using an in vivo imaging system (e.g., IVIS®). An initial imaging session before drug administration provides a precise, individualized baseline of tumor bioluminescence for each animal, effectively minimizing experimental errors arising from individual variations.
Real-Time Monitoring for an "At-a-Glance" View of Efficacy
The greatest advantage of the MHCC97-H-LUC model lies in its unparalleled real-time and dynamic monitoring capabilities. After grouping the tumor-bearing mice and administering different candidate drugs (or a placebo), researchers can track therapeutic efficacy at any point during the treatment course through repeated, non-invasive imaging, eliminating the need to wait for endpoint dissections.
Dynamic Observation of Tumor Changes: Imaging can be performed on the same cohort of mice weekly or even every few days. By comparing the bioluminescent signal intensity and spot area at different time points, the drug's effect can be visually assessed. For instance, an effective drug will cause a significant slowdown, stabilization, or even a gradual decrease and disappearance of the tumor's bioluminescent signal, clearly reflecting its cytostatic or cytotoxic effects. In contrast, the tumor signal in the control group will continuously intensify and expand. This visual evidence makes the assessment of drug efficacy highly intuitive and compelling.
Evaluating Inhibition of Metastasis: The high mortality rate of HCC is primarily due to metastasis. The MHCC97-H cell line inherently possesses a high rate of spontaneous lung metastasis, making it an excellent model for studying anti-metastatic drugs. Through whole-body imaging, researchers can not only monitor changes in the primary liver tumor but also sensitively detect the emergence of minute metastatic foci in distant organs like the lungs. Early metastatic signals, often missed by the naked eye or conventional imaging, are readily detected by BLI technology. Therefore, this model provides a clear answer to a critical question: does the new drug effectively halt the cancer cells' "expedition" while inhibiting primary tumor growth?
Quantitative Analysis for Data-Driven Decisions
Beyond providing intuitive images, modern in vivo imaging systems can perform precise quantitative analysis of the captured bioluminescent signals. This provides robust technical support for transitioning drug screening from a qualitative to a quantitative endeavor.
The system's software allows for the automatic or manual definition of a Region of Interest (ROI) over the tumor, calculating the total photon flux (photons/second) within that area. This value exhibits a strong linear correlation with the number of viable tumor cells over a wide range. By comparing these flux values before and after treatment and across different drug groups, researchers can obtain objective, quantitative data suitable for statistical analysis, thereby accurately assessing the drug's inhibition rate.
This quantitative and dynamic evaluation method significantly enhances screening efficiency. Candidate compounds that show no effect in early imaging can be quickly eliminated, allowing valuable R&D resources to be focused on more promising candidates. This not only shortens the development cycle and reduces costs but also aligns with the "3Rs" principles (Replacement, Reduction, and Refinement) of animal experimentation.
We provide high-viability, stable-luminescence, and validated MHCC97-H-LUC cells. Adopt them now to powerfully accelerate your anti-HCC drug discovery program. Click to order>>
Precision and Efficiency—A New Drug Revolution Driven by MHCC97-H-LUC
In conclusion, the combination of the MHCC97-H-LUC cell line and in vivo bioluminescence imaging has become an indispensable tool in the preclinical research of anti-HCC drugs. It transforms the "black box" of traditional drug screening into a transparent window, enabling real-time observation, dynamic tracking, and precise quantification. By establishing a visual model for pharmacodynamic evaluation, facilitating simultaneous monitoring of tumor growth and metastasis, and providing objective quantitative data, this platform is profoundly reshaping the drug discovery paradigm, empowering us to find effective weapons against hepatocellular carcinoma faster and more accurately than ever before.
References
[1] Tian, J., Tang, Z. Y., Ye, S. L., Liu, Y. K., Lin, Z. Y., Chen, J., & Xue, Q. (1999). New human hepatocellular carcinoma (HCC) cell line with highly metastatic potential (MHCC97) and its expressions of the factors associated with metastasis. British journal of cancer, 81(5), 814–821.
[12] Li, Y., Tian, B., Yang, J., Zhao, L., Wu, X., Ye, S. L., Liu, Y. K., & Tang, Z. Y. (2001). Establishment of a hepatocellular carcinoma cell line with unique metastatic characteristics through in vivo selection and screening for metastasis-related genes by complimentary DNA microarray. Journal of cancer research and clinical oncology, 127(7), 417–426.
[3] Wang, Y., Sun, Z., Peng, J., & Zhan, L. (2007). Bioluminescent imaging of hepatocellular carcinoma in live mice. Biotechnology letters, 29(11), 1665–1670.
[4] Close, D. M., Xu, T., Sayler, G. S., & Ripp, S. (2011). In vivo bioluminescent imaging (BLI): noninvasive visualization and interrogation of biological processes in living animals. Sensors (Basel, Switzerland), 11(1), 180–206.
[5] Jenkins, D. E., Oei, Y., Hornig, Y. S., Yu, S. F., Dusich, J., Purchio, T., & Contag, P. R. (2005). Bioluminescent imaging (BLI) to improve and refine traditional murine models of tumor growth and metastasis. Clinical & experimental metastasis, 22(8), 733–744.
[6] Mezzanotte, L., et al. (2017). Bioluminescence: a versatile tool for research and development. Methods and applications in fluorescence, 5(4), 042001.