More Than a Control: The Diverse Applications of the SV-HUC-1 Cell Line as a Model for Urological Diseases
Introduction
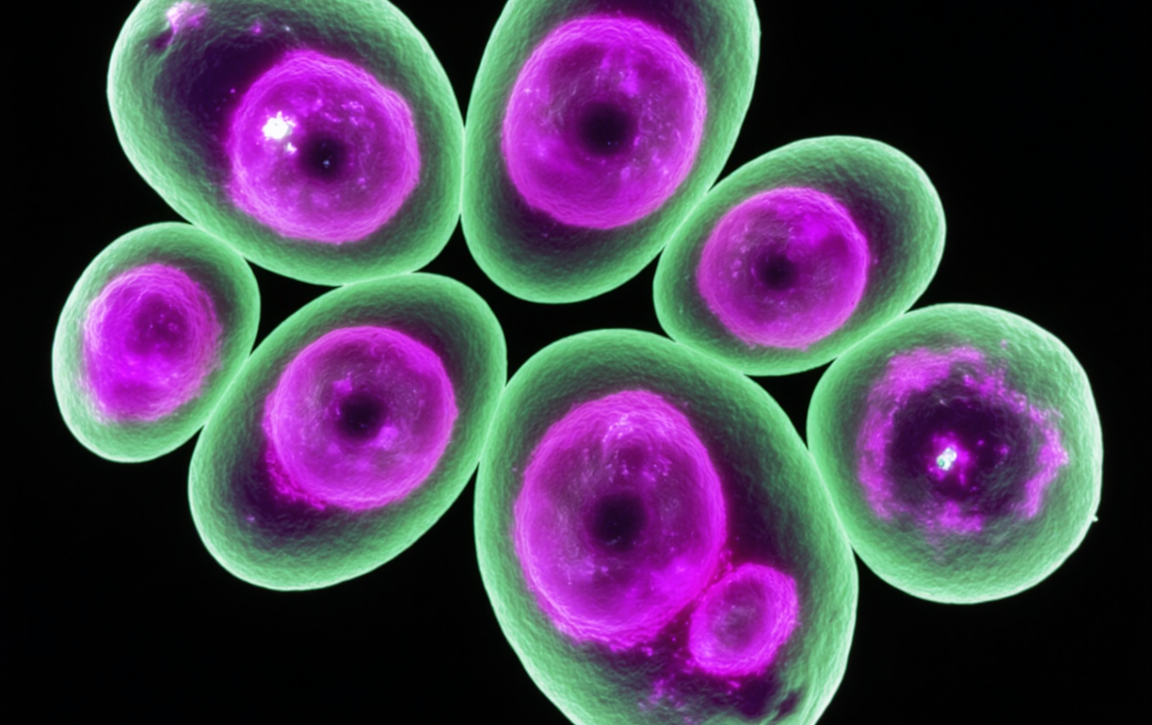
The SV-HUC-1 cell line, an SV40-immortalized human urothelial cell line, has long served as an indispensable "normal" control in bladder cancer research due to its origin from healthy tissue and stable characteristics. However, limiting its use to a mere reference for oncology underestimates its vast potential as a versatile in vitro model. As our understanding of the complexity of urological diseases deepens, researchers are expanding their focus to non-tumorous conditions. Because it effectively mimics the key biological properties of normal human urothelial cells, the SV-HUC-1 cell line is emerging as an invaluable tool for cutting-edge research in areas such as bladder pain syndrome, tissue regeneration, and environmental toxicology. It provides a novel experimental platform for elucidating disease pathogenesis and developing innovative therapies.
Move beyond a simple oncology control with SV-HUC-1 cells. Unlock vast potential in modeling urological inflammation, tissue regeneration, and toxicology today. Learn More>>
Modeling Bladder Pain Syndrome/Interstitial Cystitis (BPS/IC)
Bladder Pain Syndrome/Interstitial Cystitis (BPS/IC) is a chronic, debilitating condition characterized by pain in the bladder region and urinary urgency/frequency. Its precise pathogenesis remains unclear, but it is widely believed to involve urothelial barrier dysfunction and chronic inflammation. Establishing an in vitro model that effectively simulates the pathophysiological processes of BPS/IC is crucial for drug screening and mechanistic studies.
The SV-HUC-1 cell line offers an ideal solution. Research has demonstrated that sustained stimulation of SV-HUC-1 cells with pro-inflammatory cytokines, such as Tumor Necrosis Factor-alpha (TNF-α), can successfully induce a range of phenotypes similar to those observed in the bladder tissue of BPS/IC patients. For instance, in one study, researchers treated SV-HUC-1 cells with varying concentrations of TNF-α for 72 hours. They found that 10 ng/mL of TNF-α significantly induced a morphological shift from the typical epithelial cobblestone appearance to a spindle-like, mesenchymal form. This change was accompanied by molecular hallmarks of Epithelial-Mesenchymal Transition (EMT), including the downregulation of E-cadherin and upregulation of vimentin. Furthermore, the treated cells exhibited enhanced invasive and migratory capabilities and increased production of collagen I, which are key features of bladder fibrosis.
This SV-HUC-1-based in vitro model not only successfully recapitulates the processes of chronic inflammation-driven EMT and fibrosis seen in BPS/IC but also provides an efficient and reliable platform for screening drug candidates that could reverse or alleviate these pathological changes.
Investigating Urothelial Differentiation and Regeneration
The repair and regeneration of urological tissues represent a significant focus in regenerative medicine, particularly for clinical applications like bladder reconstruction and urinary tract repair. Stem cells, especially the readily accessible Adipose-derived Stem Cells (ASCs), are highly regarded for their multipotent differentiation potential. A core challenge, however, is efficiently inducing these stem cells to differentiate into functional urothelial cells.
In this context, SV-HUC-1 cells act as crucial inducers. By co-culturing ASCs with SV-HUC-1 cells, the microenvironment created by the urothelial cells provides essential inductive signals. One study co-implanted labeled ASCs mixed with SV-HUC-1 cells subcutaneously in nude mice. The results showed that after 2 weeks, approximately 25% of the ASCs began to express urothelium-specific markers Uroplakin-Ia and Uroplakin-II. By the 4-week mark, this proportion impressively increased to around 70%, demonstrating that direct contact with SV-HUC-1 cells successfully guided ASCs to differentiate towards a urothelial-like phenotype. Similar outcomes, where ASCs transformed into a urothelial phenotype, have also been observed in in vitro co-culture systems and experiments using conditioned medium from SV-HUC-1 cells.
These studies confirm the vital role of the SV-HUC-1 cell line in simulating the urothelial microenvironment to direct stem cell differentiation, providing a strong experimental basis and a cell-sourcing strategy for future tissue engineering approaches to repair urological damage.
Exploring Cellular Damage Induced by Environmental or Chemical Agents
The urothelium is the first line of defense, coming into direct contact with metabolic wastes and potential toxins in the urine. Therefore, assessing the potential toxicity of environmental pollutants or chemical agents on urothelial cells is critical for preventing and understanding related diseases, from chemical cystitis to bladder cancer. As a non-cancerous human cell line, SV-HUC-1 provides a more representative model for such toxicological studies compared to cancer cell lines.
Benzidine is a well-known bladder carcinogen, and understanding its mechanism of action is vital for cancer prevention. Research using SV-HUC-1 cells has investigated the effects of benzidine on normal urothelial cells. Studies have found that long-term exposure (6 days) to low concentrations of benzidine (0.001-0.01 µM) paradoxically promoted the abnormal proliferation of SV-HUC-1 cells, whereas higher concentrations (>10 µM) exhibited clear cytotoxicity. Further investigation revealed that benzidine's pro-proliferative effects may be linked to the activation of signaling pathways such as MAPK/AP-1 and PI3K/Akt. The aberrant activation of these pathways is considered an early event in cellular transformation and carcinogenesis.
By using the SV-HUC-1 cell line, researchers can clearly observe the dose-dependent effects of a chemical agent, from inducing abnormal proliferation to causing toxic damage at the cellular level. This provides direct evidence for establishing chemical safety thresholds and uncovering detailed toxicological mechanisms.
Trust SV-HUC-1 cell line for reproducible and relevant urological research. This stable human cell line is your ideal choice for everything from mechanistic discovery to drug screening. Order Now>>
Conclusion
In summary, the utility of the SV-HUC-1 cell line extends far beyond its traditional role as a control in cancer research. It demonstrates irreplaceable advantages in modeling chronic inflammatory diseases like BPS/IC, guiding stem cell differentiation for tissue regeneration, and assessing the toxic effects of chemicals on the urothelium. Acting as a bridge between basic research and clinical application, the SV-HUC-1 cell model provides robust support for deepening our understanding of the complex mechanisms behind various urological diseases and accelerating the development of novel therapeutic strategies. Future optimization and application of this cell model will undoubtedly continue to push the boundaries of urological research.
References
[1]Chuang, Y. C., Lee, W. C., Weng, S. M., Chen, C. L., Chen, Y. T., & Chiang, P. H. (2021). An experimental model of the epithelial to mesenchymal transition and pro-fibrogenesis in urothelial cells related to bladder pain syndrome/interstitial cystitis. Translational Andrology and Urology, 10(12), 4437–4451.
[2]Jiang, Y. H., Lee, C. L., & Jhang, J. F., et al. (2020). Platelet-rich plasma exerts a protective effect against hypoxia-induced apoptosis in SV-HUC-1 cells by regulating oxidative stress and the mitochondria-mediated intrinsic apoptotic pathway. Journal of Clinical Medicine, 9(7), 2243.
[3]Cao, Q., Chen, Y., & Zhang, W., et al. (2013). Differentiation of human adipose-derived stem cells co-cultured with urothelium cell line toward a urothelium-like phenotype in a nude murine model. Urology, 81(1), 227.e1-227.e7.
[4]Chen, S. C., Liao, T. C., & Chen, C. H., et al. (2018). MAPK/AP-1 pathway regulates benzidine-induced cell proliferation through the control of cell cycle in human normal bladder epithelial cells. Oncology Letters, 16(4), 5276–5284.
[5]Diensthuber, A., Bäumner, J., & Böhm, J., et al. (2024). Use of adipose-derived stem cells on decellularized bladder scaffolds for functional bladder mucosa regeneration. Stem Cells Translational Medicine, 13(7), szaf033.
[6]Alkurdi, A. F., Lim, J., & Kamaruzman, N. I., et al. (2021). Use of conditioned media (CM) and xeno-free serum substitute on human adipose-derived stem cells (ADSCs) differentiation towards urothelial lineage. PeerJ, 9, e10890.
[7]Chen, S. C., Hsu, H. H., & Chen, C. H., et al. (2018). Benzidine enhances the proliferation of bladder cancer cells through activation of the MAPK/AP-1 pathway. International Journal of Oncology, 53(6), 2617-2628.
[8]Ding, D., Geng, H., & Liu, Z., et al. (2019). Role of PI3K/Akt pathway in Benzidine-induced proliferation in SV-40 immortalized human uroepithelial cell. Translational Andrology and Urology, 8(4), 365–373.