1+1>2? The MC38 Model: Fueling the Exploration of Novel Combination Immunotherapy Strategies in Cancer
Introduction: The Future of Cancer Treatment – The Rise of Combination Therapies
While monotherapies have achieved certain successes in cancer treatment, their inherent limitations, such as drug resistance and non-responsiveness in some patients, have spurred the scientific community to actively explore combination treatment strategies. By integrating therapies with different mechanisms of action, combination therapy aims to overcome the shortcomings of single agents and maximize therapeutic efficacy, achieving a synergistic "1+1>2" effect. Against this backdrop, preclinical animal models like MC38, valued for their ability to mimic complex tumor-immune interactions, play an indispensable role in evaluating and optimizing these novel combination regimens. They provide a crucial experimental platform for screening promising drug combinations and elucidating mechanisms of synergy.
MC38 and Immune Checkpoint Inhibitors: A "Golden Partnership"
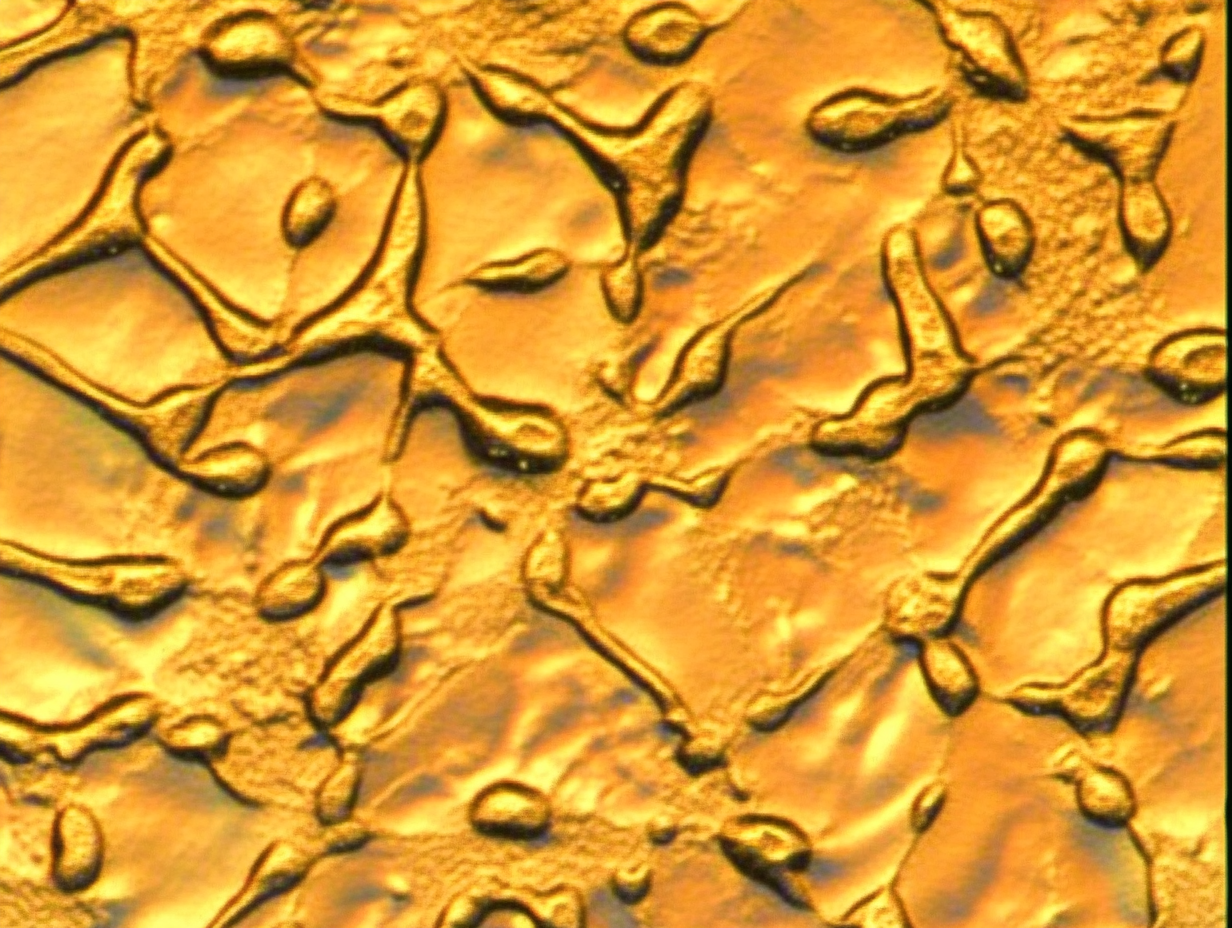
Immune Checkpoint Inhibitors (ICIs), particularly antibodies targeting the PD-1/PD-L1 axis, have become a cornerstone of cancer immunotherapy. The MC38 cell line, a colon adenocarcinoma derived from C57BL/6 mice, establishes tumors that respond well to ICI treatment, partly because MC38 cells express PD-L1. This characteristic makes the MC38 model an ideal choice for investigating the combination of ICIs with other therapies to enhance anti-tumor effects. The potential of this "golden partnership" is being extensively explored through various combination approaches.
High-quality MC38 cells help you unveil novel anti-tumor immune mechanisms.Click to check out the MC38 cell list>>
Chemotherapy was once considered immunosuppressive, but growing evidence indicates that specific chemotherapeutic agents (e.g., oxaliplatin, cyclophosphamide, 5-fluorouracil) can induce Immunogenic Cell Death (ICD) at particular doses and schedules. During ICD, dying tumor cells release various "danger signals," including the cell-surface exposure of calreticulin, ATP release, and HMGB1 secretion. These signals effectively activate dendritic cells (DCs), promoting their uptake, processing, and presentation of antigens, thereby initiating an adaptive anti-tumor immune response [1]. Furthermore, some chemotherapies can improve immune responses by depleting immunosuppressive cells (like regulatory T cells (Tregs) and myeloid-derived suppressor cells (MDSCs)) in the tumor microenvironment (TME) or by upregulating MHC class I molecule expression on tumor cells.
In the MC38 model, researchers can systematically evaluate the synergistic effects of chemotherapy combined with ICIs. For instance, mice can be treated with a chemotherapeutic drug (e.g., 5-FU, commonly used for colon cancer) followed by or concurrently with anti-PD-1/PD-L1 antibodies. Evaluation metrics typically include: 1) Tumor growth inhibition: Comparing tumor volume and weight among combination therapy, monotherapy, and control groups. 2) Mouse survival: Observing whether combination therapy significantly prolongs the survival of tumor-bearing mice. 3) Immunological mechanism analysis: Using flow cytometry to analyze the composition of tumor-infiltrating lymphocytes (TILs), especially the number, activation status (e.g., expression of IFN-γ, granzyme B), and function of CD8+ T cells; detecting changes in Treg and MDSC proportions; and analyzing cytokine levels in serum or tumor tissue. These studies help elucidate how chemotherapy creates a more favorable immune microenvironment for ICIs, leading to synergistic efficacy.
ICIs Combined with Radiotherapy: Exploring the Immunostimulatory Effects of RT and its Combination with ICIs
Local radiotherapy (RT) is a common modality in cancer treatment, primarily acting by directly killing tumor cells. However, RT has also been shown to possess potent immunomodulatory effects. RT can induce the release of tumor antigens and DAMPs, promote DC maturation and antigen presentation, and enhance T-cell recognition and killing of tumor cells. Notably, local RT can sometimes trigger an "abscopal effect," where non-irradiated distant metastases also regress, an outcome attributed to systemic anti-tumor immune activation, in which the STING pathway-mediated type I interferon response plays a key role [2].
The MC38 model is a classic system for studying RT combined with ICI therapy. Experimental designs often involve precise local irradiation of the primary tumor in MC38 tumor-bearing mice, coupled with systemic ICI administration. Researchers assess not only local tumor control and the incidence of abscopal effects but also conduct in-depth analyses of TME dynamics, such as increased CD8+ T cell infiltration post-RT, upregulation of PD-L1 expression (which may provide more targets for ICIs), and changes in immunosuppressive cell populations. Such studies can optimize RT dosage, fractionation, and the timing of combination with ICIs to maximize synergistic anti-tumor outcomes.
ICIs Combined with Targeted Therapy: Research Cases Based on the MC38 Model
Targeted therapies aim at specific molecular abnormalities in tumor cells (e.g., kinase mutations, overactivated signaling pathways) and have achieved significant success in certain cancer types. However, drug resistance is a major challenge for targeted therapy. Recent studies have found that some targeted drugs, in addition to directly inhibiting tumor cell growth, also possess immunomodulatory functions. For example, certain kinase inhibitors might affect tumor cell antigen expression, PD-L1 expression, or alter the composition and function of immune cells in the TME.
Although the MC38 cell line itself may not harbor sensitive targets for all specific targeted drugs, it can be genetically engineered (e.g., using CRISPR/Cas9) to introduce specific mutations or overexpress certain molecules, rendering it sensitive to particular targeted agents. Alternatively, combinations with targeted drugs that have broad immunomodulatory effects can be studied. In the MC38 model, researchers can evaluate whether such combination strategies can enhance anti-tumor immune responses and delay or overcome resistance to targeted therapy. For instance, studies have utilized the MC38 model to explore the effects of combining MEK inhibitors or VEGF inhibitors with anti-PD-1 antibodies, observing their impact on tumor growth, angiogenesis, and immune cell infiltration.
Combining Cancer Vaccines with ICIs in the MC38 Model
Cancer vaccines aim to induce a durable and specific anti-tumor immune response through active immunization, by delivering tumor-associated antigens (TAAs) or tumor-specific antigens (TSAs) to the immune system. However, the clinical efficacy of vaccines used alone is often suboptimal, largely due to the potent immunosuppressive network within the TME, which can limit the effector functions of vaccine-activated T cells. ICIs, by releasing these "brakes," provide a more conducive environment for vaccine-induced immune responses.
In the MC38 model, researchers can design and evaluate various forms of cancer vaccines, such as peptide-, protein-, DNA-, RNA-, or dendritic cell-based vaccines. To more accurately track antigen-specific immune responses, genetically engineered MC38 cells expressing a specific model antigen (e.g., OVA, creating an MC38-OVA model) are sometimes used. By comparing the effects of vaccine alone, ICI alone, and the combination, it is possible to clearly assess the impact of the combined strategy on: 1) Tumor control and survival: Observing whether tumor growth is more strongly inhibited and mouse survival is significantly prolonged. 2) Antigen-specific T cell responses: Using techniques like ELISpot, intracellular cytokine staining (ICS), or tetramer staining to quantify the frequency, activation status (e.g., production of IFN-γ, TNF-α), and cytotoxic function of CD8+ and CD4+ T cells specific for the vaccine antigen in peripheral blood, spleen, or tumor tissue. 3) Formation of immune memory: Evaluating whether the combination therapy can induce stronger and more durable immune memory to prevent tumor recurrence. These studies provide crucial preclinical evidence for optimizing vaccine design (e.g., antigen selection, adjuvant use, delivery systems) and combination regimens with ICIs.
MC38 in Conjunction with Oncolytic Viruses and Adoptive Cell Therapy
Oncolytic viruses are a class of viruses that selectively replicate within tumor cells, ultimately leading to tumor cell lysis. Beyond their direct oncolytic effect, a more significant role of OVs lies in their potent immunostimulatory capacity. Viral replication and cell lysis release a plethora of tumor antigens, viral PAMPs (Pathogen-Associated Molecular Patterns), and host DAMPs. These substances can activate the innate immune system, recruit and activate DCs and NK cells, and promote the initiation of adaptive immune responses. OVs can transform immunologically "cold" tumors (lacking immune cell infiltration and insensitive to ICIs) into "hot" tumors (rich in immune cell infiltration and sensitive to ICIs) [3].
The MC38 model serves as an ideal platform for evaluating the efficacy of OV-ICI combination therapy. Researchers typically inject OVs directly into MC38 tumors, combined with systemic ICI administration. By monitoring tumor regression, analyzing changes in TME immune cell infiltration (such as an increased CD8+ T cell/Treg ratio and reduced MDSCs), and detecting enhanced systemic anti-tumor immune responses, the synergistic effects of the combination therapy can be confirmed. For example, some studies have shown that in the MC38 model, oncolytic virus treatment can upregulate PD-L1 expression on tumor cells, which, in turn, creates a more favorable condition for subsequent anti-PD-1/PD-L1 therapy.
Synergistic Effects of ACT and ICIs in the MC38 Model
Adoptive Cell Therapy (ACT), particularly Chimeric Antigen Receptor T-cell (CAR-T) and T-Cell Receptor engineered T-cell (TCR-T) therapies, represents a major breakthrough in cancer immunotherapy. These therapies involve the ex vivo expansion and reinfusion of immune cells (primarily T cells) with anti-tumor activity to directly attack tumors. Although ACT has achieved tremendous success in certain hematological malignancies, its efficacy in solid tumors remains challenging, with the immunosuppressive TME being one of the primary obstacles.
Combining ICIs with ACT holds promise for overcoming these barriers by enhancing the infiltration, survival, expansion, and effector function of adoptively transferred T cells at the tumor site. In the MC38 model (especially if using MC38 cells engineered to express specific target antigens, such as MC38-Her2 or MC38-CEA), researchers can evaluate the efficacy of combining CAR-T or TCR-T cells targeting these antigens with anti-PD-1/PD-L1 antibodies. Experiments would focus on whether the combination therapy can more effectively clear established tumors, induce a more durable anti-tumor response, and prevent tumor relapse. Concurrently, the status of transferred T cells within the tumor, such as whether their expression of exhaustion markers is reduced by the addition of ICIs, would also be analyzed.
From chemo and radio combinations to oncolytic virus synergies, MC38 cells are your ideal platform for validating innovative combination immunotherapy regimens.Find out more>>
In conclusion, findings from the MC38 model are of significant reference value for guiding the design of clinical combination therapy regimens but must be interpreted with caution. Validation in more complex and clinically relevant preclinical models (such as Genetically Engineered Mouse Models (GEMMs), Patient-Derived Xenografts (PDXs), especially those incorporating humanized immune systems) is crucial. Despite these limitations, the MC38 model, with its relative ease of operation, manageable cost, and good reproducibility, remains an indispensable tool in the early exploratory and proof-of-concept stages of combination immunotherapy, helping to illuminate the path towards achieving "1+1>2" outcomes and fuel progress in the field.
References
[1] Galluzzi, L., Buqué, A., Kepp, O., Zitvogel, L., & Kroemer, G. (2017). Immunogenic cell death in cancer and infectious disease. Nature Reviews Immunology, 17(2), 97-111.
[2] Formenti, S. C., & Demaria, S. (2013). Combining radiotherapy and cancer immunotherapy: a paradigm shift. Journal of the National Cancer Institute, 105(4), 256-265.
[3] Bommareddy, P. K., Shettigar, M., & Kaufman, H. L. (2018). Integrating oncolytic viruses in combination cancer immunotherapy. Nature Reviews Immunology, 18(11), 709-722.